Holidays can put recovery at risk for alcoholics

The holiday season between Christmas and News Year's Day can be a testing time for recovering alcoholics trying to stay sober.
If alcohol has a season, it is right now.
Alcoholics feel particularly vulnerable during holidays by pointing out to them the shortfalls in their lives. It's self-delusional, of course, but many alcoholics believe that because life has failed them, it's a reason to drink.
As if alcoholics needed a reason to drink.
Some drinkers believe New Year's is coming up so it's OK to drink. But, after the holidays, they are filled with guilt and remorse.
Other heavy drinkers say the holidays mean nothing -- that when you drink, it's just another "drinking day," as they call it.
At open-to-the-public Alcoholics Anonymous meetings in Lewisburg and Sunbury on Friday, members were eager to share their experiences and talk about temptations to drink during the holiday season.
Because AA members prefer anonymity, the names of those interviewed might or might not be fictious.
Shawn, of Lewisburg, said, "At this time of year, I tend to stay away from parties where I know alcohol is being served, but if I do go I just remember that I shouldn't be drinking because I am an alcoholic. I refuse any kind of alcohol. I have to keep on my toes and pour my own drinks if I can because somebody might spike it, or someone might pass you something and say Âit's just Coca Cola' or juice. I'll watch the drinks being poured or pour it myself. Those are some of the precautions I personally have to take."
Shawn recalls being at a New Year's party one year where there was much toasting going on. "I was with another AA recovering person and everyone was raising their wine up or champagne at midnight... we raised the soda up, and a woman looked at us quite derisively, and said, ÂOh look, AA has got the soda,' and laughed at me. I remember that."
Shawn has been sober eight years.
Steve, a recovering alcoholic (sober for almost five years) from Lewisburg, said, "The holiday season isn't really a difficult time for me. I've been in the AA program for quite a few years and I think that particularly at this time of year, you should go to meetings on a regular basis. If I start to feel a little uncomfortable, I try to hit more meetings. If I have to go to parties or other social events, it's always good for me to bring along another member of AA. If I can't, I always have a way out. I drive myself, so that if I am not feeling right about a party, I can just get up and leave. I don't have to stay until the end of the party, like I used to, when I was drinking.
"At this time of year, no doubt about it, I've had thoughts about drinking," he said. "I've driven by a liquor store and thought, Âah, look at the price on that bottle. It's really cheap.'
"I always thought that if I went to a party and someone offered me a drink and I asked for a Coke, they would say, ÂWhat's wrong with you?' But what I've learned through the years is, people don't really care one way or the other."
A woman who chose to call herself anonymous (she also refused to say where she is from), said, "This is a difficult time of year. Particularly because there are more memories associated with the holidays than any other time. I don't remember what I did on March 7 or April 20. They are not prime numbers in my mind. But Christmas and New Year's have family memories, memories of people who are gone and people who are here. So it's more nostalgic. There's more emotional booby traps than we'd have at other times of year.
"My advice for alcoholics is to do the same things they do every day. Use a sponsor, go to meetings, read the literature, stay connected. I don't go around alcohol a lot. I don't have it in my house, I don't hang out with people who drink it, I don't go to places where it's served. I'll occasionally go out to dinner, but if I'm uncomfortable I don't go. Or I leave. It's important to have a way to get away if you need to.
"Alcoholism is sneaky," said anonymous. "You're never over it. It's always there. It can be arrested, but never gotten over completely and it doesn't matter how many years you've been sober. If you are an alcoholic, you think about drinking in ways that are different from other people. There is always that illusion that it's been a while or I could do this or I could have that. All the excuses. If I drink here, it wouldn't be a problem. And there are stories of people who have relapsed after really long terms and they end up dead.
"I've probably gone to 8,000 hours of AA meetings in a 25-year period since I became sober," she added, sadly. "And many people aren't here anymore. They would disappear. There is a lot of loss. A lot of recovery too, but more loss than you'd imagine."
Bob, from the Mifflinburg area is 60 days sober. He said, "this holiday season has been a difficult time of year for me. I come from a family of party people and now that I don't drink, it was a little rough at first to be with them. They did, however, support me and took away the alcohol at Christmas parties.
"This time of year, I felt more alone than I have in a long time Even being with my family, I felt alone, because when you give yourself to AA, give up the bottle after drinking for two-thirds of your life, you also give up your friends you've known all your life. Your drinking buddies."
Bob is able to deal with the season by knowing he has a sponsor to turn to. "If I have that urge, I can call him if everything went wrong at work. I would come with all kinds of excuses to stop and have that beer. ÂOne won't hurt,' I'd say to myself. But it will. So you need a support group. The sponsor will come get to you, talk to you... and the urge will usually pass."
Ben, sober for five and a half years is originally from Pittsburgh, and lives in the Lewisburg area. "In the beginning, I had a very rough time. I was a terrible person. My holidays were tougher on my family than they were on me. I was drinking, blind drunk. I wouldn't remember anything the next day. If I did remember something from the night before, it meant I didn't drink enough. My family would cry all night while I was away. It's a family illness, and if you're married with a couple of kids the emotional damage for them is 10 times worse. It should be a capital offense. I really believe that.
"Active alcoholics hurt a lot of people, mostly their families. I didn't want to, but I did. And during the holidays? Wow."
All of Ben's drinking days were tough, he said, not just Christmas and New Year's eve. "Those particular days were just an excuse to do more stupid things. I even once committed a robbery during the holidays. Crazy right? But, at least I was able to do something successfully. Even if it was criminal. By that time, I was in really terrible shape. I nearly died from alcoholism. I was as close to dying as anyone could be. I came out here to die. And I started going to meetings, got some hope...and little by little, I started getting better. Things didn't get better, but I got better.
"I was divorced. My family wouldn't have anything to do with me except my sister, who lived in this area. My three kids wouldn't talk to me. My wife divorced me. I was literally alone. I had to lose everything. I had no job. No money. But once I got here, I fell in love, got married and I'm living a good life.
John, of New Columbia, sober for less than three weeks, shared his thoughts with the Lewisburg AA group and confessed that this year provided a "new experience at Christmas. It was the first time in a long time without drinking. I didn't knock over the Christmas tree. So that was nice."
At the Sunbury AA meeting, Gene, from Coal Township, who has been sober for 30 years, said, "I'm OK now. I can deal with the amateurs out there on New Year's eve, out to prove how good a drinker they are. This is a tough time of year for newcomers. They have a difficult time with the un-wise men passing off gifts of alcohol. It's that time of year. Booze is flying around pretty loosely. We advise our newer members to stay close to the fellowship, attend plenty of meetings and keep close to your sponsors, stay away from parties, events that serve alcohol if you think you might be uncomfortable there, don't stay around people drinking alcohol."
Talking about the holidays, Gene said, "for most of us alcoholics, we'd drink every day anyhow. The holidays are just a cover up to do what we do naturally. It's the time of the year when people see us in all our natural behavior and they make allowances for us, because it is the holidays and everybody's doing it. Not knowing that we do it every day."
Gene said that on New Year's eve there would be "60 of us at someone's home celebrating in our own, non-alcoholic way. And we do this every Dec. 31. We provide a safe place for people who don't want to drink that night.
"We have a feast. It's become a tradition for this group."
But there are other ways to avoid those drinks.
Consider these New Year's eve tips courtesy of the recovering alcoholics at the Sunbury and Lewisburg area AA fellowships:
Keep a non-alcohol drink in your hand at all times.
Be prepared with what you are going to do when someone opens a beer or mixes a drink, and sticks it in your hand. Be very firm.
Remember the people you know that don't drink much or any, and seek out their company.
Keep a phone list (of sponsors if you're in AA) with you. If you have problems and you feel like you might need some help, call someone.
If you're starting to feel a little thirsty, like maybe one drink might take the edge off the nervousness, leave.
Expect questions about why you are not drinking. One suggestion: Say "doctor's orders," and leave it at that.
The AA groups we talked to for this article meet regularly in St. Matthews Church on Front Street in Sunbury and in First Baptist Church on Third Street in Lewisburg.
source: http://www.dailyitem.com
Hangover From Hell

Boozy Brits are set for the worst New Year hangover ever – thanks to new super-strength beers flooding the UK.
In the past 12 months potent foreign brews have taken the country by storm.
Supermarkets are now stocking strong overseas lagers such as 11% Kasteel Blonde, 10% La Trappe Quadrupel Strong Ale and 9% Chimay Blue.
And the new arrivals have proved a huge hit with drinkers who are lapping up the powerful imports.
But the lethal ales are set to leave Brits more worse for wear than ever on New Year’s Day as we are not used to handling the strong tipples.
Frank Sooden, spokesman for Alcohol Concern, said: “Shop-bought alcohol is now more affordable than ever. As a result alcohol at home is replacing pub culture.
“At the same time we have seen a migration away from low alcohol to stronger alcoholic drinks.
“The problem is people don’t realise how many units are contained in these new drinks.
“Because of this there will be very few people in the country who avoid the dreaded New Year’s Day hangover.” Morrisons, Tesco, Sainsbury’s and Asda are all cashing in on the craze for beers with alcohol contents pushing 10%.
Other dynamite imported drinks include 8.7% Hoegaarden Grand Cru, 8% King Cobra and 7.5% Meantime India Pale Ale.
And there are also a host of home-produced beverages following suit, including 9% Hog’s Back A Over T, 7.2% Brakspear Triple, and 6.3% Adnams Broadside Strong Original.
Even ordinarily-brewed import beers have upped the ante with alcohol contents regularly topping 5%.
But the success of the super-strength potions is now facing a backlash from ministers who fear they are damaging the country’s health.
MPs are campaigning to raise tax on beers with a particularly high alcohol content to try to stop customers turning to the dynamite drinks.
Ian Gilmore, president of the Royal College of Physicians, said: “It’s an obvious observation that drinks are getting stronger.
“There are many more of these designer beers and lagers around.
“People need to be aware that if they do drink to excess they lose control and run great risks, including getting the next-day hangover.”
source: Daily Star
Club Drugs Inflict Damage Similar to Traumatic Brain Injury

ScienceDaily (Nov. 30, 2007) — What do suffering a traumatic brain injury and using club drugs have in common? University of Florida researchers say both may trigger a similar chemical chain reaction in the brain, leading to cell death, memory loss and potentially irreversible brain damage.
A series of studies at UF over the past five years has shown using the popular club drug Ecstasy, also called MDMA, and other forms of methamphetamine lead to the same type of brain changes, cell loss and protein fluctuations in the brain that occur after a person endures a sharp blow to the head, according to recentl findings.
"Using methamphetamine is like inflicting a traumatic brain injury on yourself," said Firas Kobeissy, a postdoctoral associate in the College of Medicine department of psychiatry. "We found that a lot of brain cells are being injured by these drugs. That's alarming to society now. People don't seem to take club drugs as seriously as drugs such as heroin or cocaine."
Working with UF researchers Dr. Mark Gold, chief of the division of addiction medicine at UF's McKnight Brain Institute and one of the country's leading experts on addiction medicine, and Kevin Wang, director of the UF Center for Neuroproteomics and Biomarkers Research, Kobeissy compared what happened in the brains of rats given large doses of methamphetamine with what happened to those that had suffered a traumatic brain injury.
The group's research has already shown how traumatic brain injury affects brain cells in rats. They found similar damage in the rats exposed to methamphetamine. In the brain, club drugs set off a chain of events that injures brain cells. The drugs seem to damage certain proteins in the brain, which causes protein levels to fluctuate. When proteins are damaged, brain cells could die. In addition, as some proteins change under the influence of methamphetamine, they also begin to cause inflammation in the brain, which can be deadly, Kobeissy said.
Kobeissy and other researchers in Gold's lab are using novel protein analysis methods to understand how drug abuse alters the brain. Looking specifically at proteins in the rat cortex, UF researchers discovered that about 12 percent of the proteins in this region of the brain showed the same kinds of changes after either methamphetamine use or traumatic brain injury. There are about 30,000 proteins in the brain so such a significant parallel indicates that a similar mechanism is at work after both traumatic brain injury and methamphetamine abuse, Kobeissy said.
"Sometimes people go to the clubs and take three tablets of Ecstasy or speed," Kobeissy said. "That may be a toxic dose for them. Toxic effects can be seen for methamphetamine, Ecstasy and traumatic injury in different areas of the brain."
About 1.3 million people over the age of 12 reported using methamphetamine in the previous month, according to the 2006 National Survey on Drug Use and Health. In 2004, more than 12 million Americans reported having tried the drug, the survey's findings show.
People often think the effects of drugs of abuse wear off in the body the same way common medications do, but that may not be the case, Gold said.
"These data and the previous four years of data suggest some drugs, especially methamphetamine, cause changes that are not readily reversible," Gold said. "Future research is necessary for us to determine when or if methamphetamine-related brain changes reverse themselves."
Gold and Dennis Steindler, director of UF's McKnight Brain Institute and an expert on stem cells, are planning studies to find out if stem cells can be applied to repair drug-related brain damage.
UF researchers are also trying to uncover all the various ways drugs damage and kill brain cells. During their protein analysis, researchers discovered that oxidation was damaging some proteins, throwing the molecules chemically off balance.
"When proteins are oxidized they are not functional," Kobeissy said. "When proteins are not working, the cell cannot function."
Neurologist Dr. Jean Lud Cadet, chief of the molecular neuropsychiatry branch of the National Institute on Drug Abuse, said analyzing proteins is important to understanding how drugs such as methamphetamine affect the brain.
"I think saying the results of methamphetamine abuse are comparable to the results of a traumatic brain injury is a new idea," Cadet said. "I agree with (the findings). Our own work shows that methamphetamine is pretty toxic to the brains of animals. In humans, imaging studies of patients who use methamphetamine chronically show abnormalities in the brain.
"Abuse of methamphetamine is very dangerous."
This research was presented at a Society for Neuroscience conference held recently in San Diego.
Adapted from materials provided by University of Florida.
Study finds addicts' brains wired differently
Authors say research supports notion that addiction is a disease
Drug or alcohol abusers who relapse, even after long periods of abstinence, are often reviled as too weak or undisciplined to straighten themselves out.
But a UNC Chapel Hill psychologist has found evidence that suggests, in fact, that addicts' brains may be wired in a way that makes them more prone to give in to temptation.
The research, published in the December issue of the Journal of Neuroscience, provides further evidence that addiction is a disease, not a character flaw, says Charlotte Boettiger, an assistant professor of psychology at UNC and lead author of the paper released Tuesday.
"It wasn't that long ago that we believed schizophrenia was caused by bad mothers and depression wasn't a disease," Boettiger said. "Addiction is maybe just a couple of decades behind."
What they did: Boettiger and colleagues peeked inside the brain to see how brain function might be different in a substance abuser.
The study, conducted while Boettiger was at the University of California at San Francisco, used imaging technology to take pictures of sober alcoholics' and nonalcoholics' brains as they chose between immediate and delayed rewards. Alcoholics chose the quick payoff almost three times more often.
What they found: Scans showed that the most impulsive subjects -- most but not all of whom had a history of alcoholism -- had reduced activity in an area of the brain that helps assess rewards and increased activity in other sections of the brain associated with judgment and decision-making. The differences suggest that some addicts may have impaired ability to think through a decision, Boettiger said. Blood tests implicated a variant gene.
What it means: More study is needed, but Boettiger said the findings suggest new treatment approaches for addiction. Drugs for early-onset Alzheimer's disease and Parkinson's disease target the same regions of the brain, so those medicines may also be useful for alcohol or drug addiction.
source: JEAN P. FISHER
(Raleigh) News & Observer
http://www.charlotte.com/
Let's not go soft on hard drugs

We need a thoughtful approach to tackling our so-called cocaine crisis rather than overhyping the problem or opting for legalisation, argues Patrick Kenny
It is clear for all to see that Ireland has a growing cocaine problem which we must face in a sensible and coherent manner. But in the process of tackling the problem, we must steer a careful path between two major mistakes that would make the situation worse.
The first mistake is that of normalising the problem by hyping its prevalence. The recent Prime Time Investigates programme grabbed the headlines with its findings that cocaine traces can be found in most pubs and nightclubs. But that is a long way from showing that most individuals take cocaine. If we create the impression that "everyone" takes cocaine when they clearly don't, and if we communicate the idea that cocaine use is now the expected behaviour for young people, we can make the problem worse because of the powerful effect of social norm perceptions on human behaviour.
The second, and even greater, danger is to indulge in poorly thought-out policy reactions that will have the ultimate effect of making the problem worse. That's why arguments about legalising cocaine and other drugs, must be rejected.
One of the arguments for legalisation is that state controls would put the crime lords out of business. But there is absolutely no evidence for this. Do we really believe that the gangs who have made millions, and who are prepared to kill to protect their narcotic empires, will simply walk away and retire?
At what age should children be allowed to buy legal cocaine? One study released earlier this year indicated that 40 per cent of Irish 15-year-olds have dabbled in illegal drugs. Should cocaine be legal for kids of this age? Unless we make cocaine more freely available than alcohol and tobacco, and place no age limits on it, a black market for underage cocaine will remain. In such a scenario, what's to stop our drug lords killing each other to capture the teen coke market? And what if the cocaine magnates diversify into other banned substances, creating a new, expanded market where they won't have to compete against the local cocaine-selling pharmacy? Do we really want expert drug pushers pursuing our teenagers in this way? What about the cost of legal cocaine? What's to stop the criminal gangs from undercutting the price of legal cocaine?
But even if, in some alternative reality, the decriminalisation of cocaine would reduce crime, we still face a choice between two major evils and must ask ourselves which of them is the lesser: gangs wiping each other out or the prospect of even greater drug abuse and death in the rest of the population due to decriminalisation?
Legalising cocaine would inevitably increase drug consumption levels and with them, drug-related tragedies because the law plays a significant role in influencing human behaviour. Of course, it is peers that have the most intensely powerful impact on our behaviour, precisely because friends help to establish the social norms. But if this potent peer pressure has already led to a significant cocaine problem, how much greater would our problem be if the State endorsed cocaine?
Britain, in taking a softer approach to marijuana, has seen a 22 per cent increase in hospital admissions of cannabis users. The Netherlands, with its enlightened drugs policy, has seen a dramatic rise in heroin use since soft drugs were legalised. Meanwhile, Sweden, with some of the toughest drugs laws has Europe's lowest consumption rate.
After the recent cocaine-related death of Kevin Doyle, 21, of Waterford, his family said that they "sincerely hope that no family has to suffer the pain that we are going through".
Can we really believe that a dangerous experiment with legalised cocaine would help their wish to come true?
Patrick Kenny is a lecturer in marketing in the Dublin Institute of Technology.
source: http://www.independent.ie/
Personal alcohol testers: worth the price?

Experts doubt the effectiveness of consumer-grade breathalyzers
Holiday partygoers who plan to drink should beware: A public safety campaign will mobilize extra law enforcement from now until Jan. 2. That means some partiers will get designated drivers, while others will look for alternate transportation. And for those who plan to drive: Some marketers are touting personal breathalyzers that say they help drivers test their limits before they get behind the wheel.
Breathalyzers have been used by law enforcement agencies for years to test blood-alcohol levels, which can be detected by measuring the amount of alcohol in a person's breath. Similarly, some consumer breathalyzers, which can cost from $16 to $1,000 and range from small key chain gauges to handheld detectors, claim to provide an accurate digital blood-alcohol-content reading, or BAC, in seconds.
Massachusetts State Police captain Daniel Wicks says that if these devices work, "they might be a good aid in educating and informing the driver."
Others caution drivers against using them. "These consumer breathalyzers are interesting and may make you more aware of your BAC, but there's no evidence to show that it's an effective way of keeping people from driving while impaired," says Linda Degutis, an associate professor at Yale University who studies alcohol interventions and policies. "In fact, they may give people a false sense of security."
To be sure, consumer breathalyzers, while compact and relatively easy to use, do not give legally admissible results. Expensive equipment that provides such results requires regular calibration and maintenance and must be operated by certified personnel. And even the validity of those tests is regularly challenged in court.
When in the market for a consumer breathalyzer, the more expensive models may be better. Mac Forrester, owner of Intoximeters Inc., a St. Louis maker of equipment for industrial applications such as workplace substance abuse testing, says that mass market alcohol screeners using semiconductor chips are not as stable as those that use infrared devices or fuel cell sensors. The inexpensive chips are prone to false positives, which even can be caused by the acetones in a marathon runner's breath, detected after burning fat during exercise.
"These consumer breathalyzers sell because of the price and ignorance of the purchasing population," Forrester says.
Conversely, he said more expensive models, which use more reliable technology such as infrared or fuel cell technology, yield more accurate results. These professional-level models, which range from $400 and up, can be purchased by the general public.
No matter which device you choose, Barbara Harrington, state executive director of Mothers Against Drunk Driving, says the organization does not recommend monitoring blood-alcohol content and then making a decision about whether to get behind the wheel. Instead, she says people should make a plan for sober driving before drinking begins.
"Some folks who drink are searching for that sweet spot between sobriety and being illegal at .08," says Harrington. "But it doesn't make sense that a person can manage drinking by testing themselves and making a judgment based on test results."
source: The Boston Globe
© Copyright 2007 Globe Newspaper Company.
Doctors may soon offer what alcoholics need (if not what they want)

Addiction medication and sage advice could be dispensed from a physician's office.
British songstress Amy Winehouse, who croons "no, no, no" to rehab, has a lot of American company this time of year -- both in her heavy-drinking ways and her unwillingness to spend weeks in a specialized facility to get sober.
But experts say there may be new hope for rehab refuseniks like Winehouse and an estimated 5.7 million alcoholics in the United States who are not in treatment -- hope that could be as close as the family doctor.
New research and a growing arsenal of medications have set the stage for a major shift in the treatment of alcoholism, from specialized clinic to the "primary care office setting," the Journal of the American Medical Assn. reported in its Dec. 5 issue.
But if the promise of "office-based" treatment of alcoholism is to become a reality, the nation's 337,000 general-practice physicians -- and the systems within which they work -- will have to undergo some transformation themselves, addiction experts say.
Doctors must overcome their reluctance to broach the subject of drinking and learn how best to intervene when they suspect alcoholism. Medical practices may need to add staff to help counsel recovering patients. And insurance companies and federal insurance programs will need to be persuaded to reimburse patients for medication that can be costly and to pay physicians for taking on a new role in patients' care.
Several new drugs are making office-based treatment a realistic prospect. In April 2006, a monthly injectable form of the drug naltrexone won approval from the Food and Drug Administration. Marketed as Vivitrol, the new formulation of a long-available drug can be started after only four days of abstinence and appears to cause less nausea than pills taken daily -- features that make it easier for patients to start and stay on the treatment. It joined two other medications approved to curb alcohol cravings.
Evidence is growing for the effectiveness of these and other addiction medications, such as the anti-convulsive drug topiramate, which, although not FDA-approved for this purpose, is also widely prescribed off-label to help alcoholics stay away from drink. And more FDA approvals for drugs that treat alcohol dependence are on the horizon.
At the same time, studies published this year underscored the effect that a few frank words from the doctor can have on patients whose drinking appears to have become excessive.
These developments could be the "tipping point" into a new era of alcohol treatment, says Mark Willenbring, director of treatment and recovery research at the National Institute on Alcohol Abuse and Alcoholism. With new confidence in their powers of persuasion and new pharmaceutical tools in their black bags, primary care physicians -- who have been notoriously shy of confronting patients about their drinking habits -- may grow more willing to flag an alcohol problem, offer medication and dispense advice during routine office visits, Willenbring says.
In turn, as patients grow more confident that they can curb their drinking without the time, expense and stigma of a stay in a clinic, more will likely step forward for help.
Parallel with depression
"In many ways, we are with alcoholism where we were with depression 30 years ago," Willenbring says. As a new generation of antidepressants came to market in the early 1980s, physicians on the front lines of patient care grew more attentive to the signs of depression and more willing to treat it. Patients with protracted bouts of blue mood turned to their family doctors for help in increasing numbers.
In the process, depression was transformed from a highly stigmatized mental illness that was rarely treated before a suicide attempt or outside a psychiatric hospital to a condition for which 80% of patients turn first to a general medical practitioner.
A similar shift in the treatment of alcohol-related disorders won't happen overnight, Willenbring says. But with 19.5 million Americans thought to have alcohol-related disorders in 2006, and only 1.6 million getting specialized treatment, he says, "we have to start thinking creatively about how to provide more accessible, appealing and creative options" to encourage patients with drinking problems to get the help they need before they hit the skids.
Experts warn, however, that as general-care physicians armed with medications shoulder a greater role in treating alcohol dependence, patients and public officials must ensure that the sickest patients do not suffer in a rush to treat alcoholism more economically.
In that regard, not all experts see depression treatment as an encouraging example. Medication has worked wonders for many depressed patients. But a study published in 2001 found that only about one-quarter of depressed patients seeing a general practitioner got appropriate care. Meanwhile, insurance companies keen to reduce spending for depression care have limited patients' access to costly psychotherapy, despite studies showing that patients improve most when such therapy is paired with medication.
As anti-alcoholism drugs show gains in effectiveness, many fear that insurance companies and federally supported programs will rely largely on medications and the brisk medical management of primary-care doctors.
That, they fear, could deny alcoholics who need the extra support of intensive rehabilitation the care they need to quit.
"You'd have to be naive not to be a little concerned that that will happen," says Mitchell Karno, UCLA's alcohol treatment researcher.
Doctors, too, will have to make changes if this new era of "office-based" alcohol treatment is to become a reality, experts say -- and some aren't convinced that the changes will easily happen.
"It's a vision that has some benefits to it, but it's not a done deal at this point," says Richard Rawson, associate director of UCLA Medical School's Integrated Substance Abuse Programs.
Rawson observed one crucial obstacle when he tried to launch a pilot program in which U.S. primary care doctors would screen patients for risky or excessive alcohol use and provide "brief interventions" intended to get those with problems to quit or reduce their alcohol consumption.
In all, the prescribed screening and intervention initiative would have taken physicians 10 minutes, Rawson says. He approached five institutions in an effort to recruit support.
None bit.
"What we hear over and over again is, 'Look, we have seven minutes to do whatever it is we're going to do. To take five minutes to do screening and then another five to do a brief intervention on this one dimension of health problems is just not in the cards,' " Rawson says. "I don't think we're at a point where we can just dump it all in the laps of primary care docs."
Rawson adds that in addition to physician training, other things would also have to change to account for the new demands -- such as systems of payment, insurance reimbursement and the office structure of general care practitioners.
Another obstacle experts see: Doctors are generally wary of challenging patients in matters that involve emotionally charged personal habits such alcohol consumption as well as smoking and obesity. And patients, in any case, almost always lie about their habits.
Physicians frequently hesitate to raise the question unless a patient is showing clear evidence of alcohol-related damage -- including impaired liver function, high triglycerides or bloated red blood cells. "It's like, 'Don't ask, don't tell,' " says New York internist Dr. Steven Lamm, who has successfully treated a number of patients with medication, including the monthly injectable version of naltrexone. That's especially been the case, he adds, because of the perceived paucity of medical treatments they have to offer. "What are you going to do about it? Send them to Alcoholics Anonymous?" he says.
Change is in the air
In the new climate, such reluctance might change.
As pharmaceutical companies launch new drugs -- and new marketing campaigns for them -- doctors will grow more assertive about raising the issue, says UCLA geriatrician Dr. Alison Moore, who sits on a panel at Willenbring's NIAAA that reviews the effectiveness of alcoholism treatments.
But, Moore adds, in addition to writing prescriptions for new drugs, physicians also had better learn new scripts for how to talk to patients about their alcohol problems and where to refer them if they need more help than a pill or an injection can provide.
"They're better than nothing," Moore says of the available medications. "But I don't see them as wonder drugs." They don't work for all patients, and even when they do, patients frequently relapse, she adds.
A new era in alcohol treatment may also bring new definitions of sobriety, as well, experts say. Programs such as Alcoholics Anonymous, as well as most of those who treat alcoholism, have always drawn a clear line between sober -- completely abstaining from alcohol -- and alcoholic.
As alcohol treatment grows more accessible, however, a wider range of patients -- including those who are not alcohol-dependent, but who endanger their health by drinking to excess -- are expected to come forward for treatment. For these patients, support groups like Alcoholics Anonymous may be less relevant than newer groups such as SMART Recovery and Rational Recovery, less ubiquitous than AA, which emphasize a goal of moderation in drinking.
In January, the NIAAA will launch a print- and Web-based self-help program called "Rethinking Drinking," aimed at a wide range of drinkers, including those with what Willenbring calls "a mild form of alcohol dependence."
The emergence of these alternatives to AA is certain to reignite a long-running debate over what goals alcoholism treatment should embrace. And it will likely spark efforts to define more broadly the range of patients who have a drinking problem, as well as those who could benefit from preventive or early treatment.
UCLA's Mitchell Karno says that patients and their family doctors will likely work out their own solutions. "People will seek out the level of treatment that's going to match their need," Karno says -- whether it's eight weeks in rehab, or a pill, an encouraging word from the doc and a self-help book.
Between strict abstinence and a safer level of drinking, Karno says, "it will be up to physicians and patients to choose how they're going to negotiate that tension."
source: Los Angeles Times
melissa.healy@latimes.com
Four Pillars plan totters on two: harm reduction and police

Among the many problems with Vancouver's failing Four Pillars approach to the grotesque addiction problems in the Downtown Eastside is that it has spawned the Not-in-Anybody's-Backyard movement.
It now seems impossible for municipalities like Richmond, Coquitlam, Gibsons, or Keremeos to even consider proposals for abstinence-based treatment centres without NIABY proponents raising red herrings such as Vancouver Mayor Sam Sullivan's support for providing free heroin to addicts or Senator Larry Campbell's support for reforming drug laws.
They even question the fact addiction is a disease, not a choice.
Small wonder.
The Four Pillars plan totters on only two -- harm reduction (which includes the safe injection site, the ever growing distribution of free needles, methadone and possibly free heroin) and the best enforcement Vancouver police can muster without completely abandoning the rest of the city.
It hasn't made a dent in the nightmarish scene at Main and Hastings or the lives of the hundreds of addicts who congregate there.
No one wants that replicated in their community.
However, that begs the issue of treatment.
As this week's series in The Vancouver Sun makes clear, alcoholism alone affects thousands of Canadians. It also makes it clear that tens of thousands of Canadians have recovered with treatment. And while the series focused on alcoholism, clinicians don't differentiate between them and drug addicts. They are unequivocal.
Addiction is a neurological disorder for which the only cure is abstinence and that means recovery is a process that takes years and often many attempts.
"There is no place for controlled substance abuse in addiction. Period," said Dr. Graeme Cunningham, associate clinical professor of psychiatry and director of the addiction division of an Ontario health centre.
For years, Dr. Douglas Coleman along with other board-certified addictions physicians have been saying the same thing in Vancouver. But they're rarely heard above the din of harm-reduction proponents and others who suggest drugs aren't addictive, rather a symptom of poor living conditions or some other disorder.
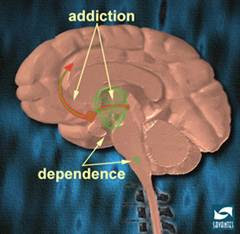
Medical experts like Coleman define addiction as a war between two parts of the brain. The forebrain, which controls our intellectual or rational understanding, is not able to keep the mid-brain, the emotional centre, in check.
Addicts are, in Coleman's words, people who continue to use drugs or alcohol despite knowing the consequences are episodes of loss of control and an ongoing preoccupation with getting that next drink or fix.
They drink or use drugs knowing full well it will impair their judgment.
That's what they want.
As Coleman says, "There's not a respectable addict in this country who would say, 'No, I think I've had enough.'"
Abstinence is the only proven cure, which is why Alcoholics Anonymous, Narcotics Anonymous and Turning Point, which is proposing a 32-bed facility in Richmond, insist on it.
Each week across Metro Vancouver, there are 700 Alcoholics Anonymous and Narcotics Anonymous meetings. That's 100 meetings a day in different neighbourhoods attended by doctors, lawyers, clerics, truck drivers, airline pilots, journalists, and every other kind of person you can imagine.
That's why it makes sense to not put recovery services in the midst of Vancouver's chaotic, drug market.
It's like holding Weight Watchers' meetings next door to a chocolate shop.
Harm-reducers have all but convinced us that some people can't be cured because there is too much wrong with them -- mental illness piled upon multiple addictions.
Email to a friendEmail to a friendPrinter friendlyPrinter friendly
Font:
So, who wants them in their neighbourhood?
But Coleman contends everyone has the potential to abstain and recover. To suggest harm recovery is the best we can do, he says, is a death sentence.
Even NIABYs don't oppose treatment. They simply want it far away from them, which has proved an attractive idea to urban politicians, especially Vancouver-Burrard MLA Lorne Mayencourt.
His non-profit, New Hope Recovery Society has taken over Baldy Hughes, an abandoned U.S. military base 35 km from Prince George. Based on the village model of San Patrignano, Italy, and the principle of abstinence, the first recovering addicts moved in earlier this month.
Last spring, The Sun's Jonathan Fowlie visited San Patrignano where addicts spend an average of three to four years recovering.
One resident told him that when she went home for a short visit, "It was strange. I felt like a Martian. I felt it was a world that wasn't mine anymore."
That's why addictions specialists refer to wilderness camps as "the Greyhound cure." It doesn't fully address the reasons addicts craved impairment in the first place.
So, what we're left with is this:
We can maintain the status quo, pouring millions of dollars into the Downtown Eastside and pretending that two pillars are four.
We can pack addicts off to the hinterlands and hope they don't come back as Martians.
Or, we can accept the medical evidence that recovery is a slow, hard process that's made easier if people get needed services in their own communities where, unimpaired, they can rebuild and resume their lives.
dbramham@png.canwest.com
source: Daphne Bramham, Vancouver Sun
Published: Friday, December 21, 2007
© The Vancouver Sun 2007
System could monitor Broward drug abuse

A pilot program based in Broward County would help police and doctors track prescriptions.
Broward County, scene of the most famous prescription-drug overdose this year, might become the testing ground for a new database aimed at curbing doctor-shopping.
Florida legislators are proposing a pilot program that would create a computerized system to track the prescriptions that are requested, written and filled in Broward for some of the most addictive medicines.
Certain prescription drugs -- including those like Oxycontin, Vicodin and Xanax -- were implicated in more than 300 Broward deaths last year.
Earlier this year, celebrity Anna Nicole Smith died during a stay at the Seminole Hard Rock Hotel & Casino near Hollywood. An autopsy concluded that a lethal mix of at least nine prescription drugs caused her death.
While high-profile cases like Smith's -- and that of conservative pundit Rush Limbaugh, who admitted an Oxycontin addiction in 2003 -- grab headlines, supporters of stricter prescription monitoring say the abuse of legal medication is causing a growing number of deaths, arrests and emergency-room visits. In recent months, they say, out-of-state visitors have been shopping for Florida doctors, creating a form of prescription-drug tourism.
''It's a serious problem,'' said state Rep. Jack Seiler, a Wilton Manors Democrat and House sponsor of the proposal. ``And if you think for a moment those costs aren't being borne by the taxpayer, you're wrong. The North Broward Hospital District, the South Broward Hospital District, the courts, the jails -- those are all things that we pay for.''
Supporters say they will continue to push for a statewide program as in years past, but want to present the one-county pilot as an alternative.
Opponents say most tracking systems do little to reduce abuse and might discourage doctors from writing prescriptions for those who need them.
''If doctors know they're being watched, then they won't do as much,'' said David Brushwood, a professor at the University of Florida's College of Pharmacy. ``It's like going through a speed trap. When people go through a speed trap, we want them to slow down to the speed limit. We don't want them to slow down below the speed limit because that's dangerous.''
OVERDOSE DEATHS
Statewide, prescription drugs caused more than twice as many overdose deaths last year as illicit drugs, such as heroin or cocaine, said Bill Janes, director of the state's Office of Drug Control. Drugs like Oxycontin, Vicodin, Valium and Xanax were involved in more than 500 deaths in Broward and Miami-Dade counties.
''There's something more socially acceptable in taking a prescription medication than taking cocaine on the street,'' said Dr. Jeffrey N. Bernstein, medical director of the Florida Poison Control Center and an attending physician at Jackson Memorial Hospital. ``It's easier to go to a doctor and pretend you have back pain and try to get a prescription for a painkiller than it is to go into a bad neighborhood and look for an illegal drug.''
The number of cases in Broward's drug court involving doctor-shopping has at least doubled in the past few years, said Judge Marcia Beach.
A decrease in the number of cocaine arrests has helped prevent a backlog, she said. But Beach said many prescription-drug patients have built up a high tolerance for the drugs and need more-expensive care.
''It's difficult for them to detox,'' Beach said. ``And it's more difficult for them to succeed on an outpatient basis. . . . Many of them require residential treatment.''
The proposed $1.6 million Broward database would keep a record of a patient's prescriptions and could be accessed by doctors, pharmacists, patients, law-enforcement agencies and the Agency for Health Care Administration. It would be funded privately and with federal grants and would be designed to look for people who are ''doctor-shopping,'' that is, visiting multiple doctors in search of duplicate prescriptions.
''If they go to one ER, then 30 minutes later they go to another ER, then 30 minutes later they go to another ER -- that's not a person in real pain,'' said Dr. Nabil El Sanadi, chief of emergency medicine for Broward Health. ``If they were tracked in that database, we could see it better.''
About 35 states have passed legislation to create a monitoring system, and at least 24 are in use. Florida is the largest state without one, which worries law-enforcement and drug-abuse experts who say they have seen a growing number of prescription-drug tourists.
''They find it cheaper to come to Florida, stock up, have a nice vacation and head back and have enough pills to feed their habit and to sell and pay for the trip,'' said Jim Hall, director of the Center for the Study and Prevention of Substance Abuse at Nova Southeastern University, which has a partnership with the Commission on Substance Abuse of the United Way of Broward County.
BUY AND SELL
Sgt. Lisa McElhaney, of the drug diversion unit of the Broward Sheriff's Office, said that in the past couple of months, the BSO has found at least 600 people trying to buy prescription medications in Broward to sell in other states.
''Florida has become a source state for prescription-drug seekers,'' she said.
Lawmakers have tried to create a statewide database for the past five years -- with powerful backers, including former Gov. Jeb Bush.
Concerns about patient privacy and how to pay for the database have stalled previous attempts at monitoring.
Brushwood questions the effectiveness of such systems. Many don't include enough personal information to tell whether prescriptions were issued to one person or several with similar names, he said. The systems could be circumvented with fake IDs.
''The question is: Does it reduce diversion and substance abuse?'' Brushwood said. ``I don't think it does.''
Opponents of the one-county Broward proposal argue that people would just move on to Miami-Dade or Palm Beach.
''Limiting it to just Broward won't capture the kinds of data and control substance abuse like we'd like to see,'' Broward Mayor Lois Wexler said. ``It's too easy to cross county lines here, so I would encourage the program to be regional.''
Bernstein, of the Florida Poison Control Center, said that the details need to be worked out, but that without better tools, doctors can be left relying on instinct.
''Nobody wants to see anybody in pain,'' he said. ``But you have no way to know that he's been to five other ERs in town.''
source: miamiherald.com
Housing provides security, solace

Mamie Medrano, 44 and a recovering alcoholic, has struggled to find safe, affordable housing.
Living in shelters and then with relatives, she drifted in and out of homelessness for years, taking her young daughter with her.
Their lives changed for the better in November 2001, when the pair moved into The Holland Apartments in Roseland on the city's far South Side.
The building is owned, managed and operated by Mercy Housing Lakefront, a non-profit that helps provide housing, job training and other services to previously homeless residents.
The organization, which serves some 2,000 people in 15 buildings throughout Chicago, is funded in part by the Corporation for Supportive Housing. Both are supported by Chicago Tribune Holiday Giving, a campaign of Chicago Tribune Charities, a McCormick Tribune Foundation fund.
Medrano said her spacious, two-bedroom apartment brings her the type of peace one can only feel in the knowledge one has a safe, clean place to live. It's allowed her to focus on her other problems, to attend Alcoholics Anonymous meetings and work each day to fight her addiction.
'I can get sober,' she said. 'But to stay sober, that takes a lot of work for me.'
It's been hard to stay clean, and her resolve has been tested many times.
'I've been through so much,' she said. 'I grew up real fast.'
Medrano started sipping alcohol in her bedroom when she was 11. Now, when she's tempted to drink, she knows how to fight the urge.
Standing inside her apartment, her brow damp with sweat from cooking dinner, she's finally on firm ground.
'I thank God,' she said. 'I'm stable now.'
Her daughter, 9-year-old Mandi Walker, a playful girl who greets visitors with a hug, is thriving in the apartment, saying she's happy to have her own bedroom.
'It feels great,' she said, playing cards in the living room next to a brightly lit Christmas tree.
Residents living in other Mercy-run buildings echo the same pride.
It's been two years since Freeman Rufus moved into Wentworth Commons, also in Roseland.
He needed a place to stay after asthma forced him to quit his job as a meat cutter.
Rufus, who punctuates nearly every sentence with a hearty laugh, lived for a time in a shelter and spent a couple of nights in the lobby of a police station, anything to get out of the cold.
Wentworth Commons has not only provided him with shelter, but also has given him an added sense of purpose. Rufus, 56, spends much of his time volunteering, participating in voter registrations drives, neighborhood cleanups and other programs.
'I never imagined I'd be doing all of this,' he said, thumbing through a wall calendar that's nearly full. 'It's opened up the door to so many things.'
Rufus revels in the comforts of his small apartment. But like many residents here, he looks forward to when he can move and make room for the next tenant. Until then, he'll relish every day here.
'This is my family,' he said of the other residents.
Each tenant in Mercy's buildings has a case manager and property manager to help them take responsibility for paying rent, among other goals. In many cases, tenants are employed on site, some as custodians and desk clerks.
Part of Mercy's goal is for the housing units to blend into - and in some cases improve - the quality of the surrounding area.
Residents are invited to use the buildings' meeting spaces and computers. Tenants are encouraged to take ownership of the communities in which they live, which is why there is such a push to volunteer.
Organizations like Mercy Housing Lakefront couldn't operate without funding from other groups, such as the Corporation for Supportive Housing or CSH.
CSH, a national organization with an office in Chicago, doesn't build homes. Instead, it helps other groups formulate plans to build new housing units or convert other buildings into permanent homes by providing both money and guidance.
'Our role is to help organizations create this type of housing,' said Katrina Van Valkenburgh, the Corporation's associate director.
Peggy Haywood, 42, wanted to give her daughter and grandson a safe place to live. She and her family moved into Wentworth Commons about five months ago.
Haywood used to work for an attorney in a law firm. But when he left, she was out of a job. She now works as a clerk for another of Mercy's housing units.
'I'm very pleased with what I have,' she said of her apartment. 'It's quiet, secure. All of the apartments are well-built. It's my own little sanctuary.'
source: By Jo Napolitano
Chicago Tribune
jnapolitano@tribune.com
Copyright © 2007 Chicago Tribune, All Rights Reserved.
The high cost of alcohol abuse
'No. 1 problem substance in Canada'
Do you ever drink to escape from your worries or troubles?
If you answer yes, you might need help.
The message this time of year in the glitzy holiday cocktail guides is: Drinking is good. Drinking is glamorous. Sexy, desirable people drink.
Across Canada, per capita consumption of our favourite legal psychoactive substance has increased more than 11 per cent over the past decade.
People are drinking more frequently, more heavily, and more women are starting to drink like men. Women who pick up a bottle on the way home from work. Women who don't have sober sex. Teachers and administrators and nurses and doctors' wives who sit in group therapy sessions in rehab with former sex workers and drug addicts fighting to get their children back, wondering, "How did I get here?"
Meanwhile, a prosperous economy, an increase in the availability of alcohol nationwide, longer drinking hours, more concentrated hot spots where bars compete and offer discount drinks and sometimes less-than-strict serving practices are fuelling the consumption, experts say.
And as our bond with booze grows, so too will hospital stays for alcohol-related violence, road crashes and attempted suicides; cirrhosis of the liver and drink-related cancers that follow alcohol's path from the lips and mouth down through the body's many systems.
In 2005, there were 25,194 alcohol-related injuries and illnesses in B.C. needing hospitalization, compared with 4,817 related to illicit drug use. A Canadian study found that 42 per cent of those with violent injuries had a blood-alcohol level above the legal limit.
"Alcohol has always been, and will continue to be for a long time, the No. 1 problem substance in Canada for men and women," says Gail Malmo, of the Aurora Centre at B.C. Women's Hospital and Health Centre. The largest women's-only addictions treatment centre in B.C. treats about 300 patients a year.
"We like to think of it as 'other' people. By focusing on the heroin users and the cocaine users you can keep addiction away from you," Malmo says.
A drinker's response to a second question -- Do you drink to build up self-confidence? -- can also be telling.
If you answer yes to this question, and if you also answered yes to the question about drinking to escape your worries, chances are you are an alcoholic. That's according to a recognized test used by Johns Hopkins University Hospital in Baltimore.
Despite warnings that alcohol use and misuse is substantial, Canada has no national drinking guidelines.
"If you just tell somebody, drink responsibly, what's it mean? We have no idea. We've never told anybody what it means," says Doug Beirness, manager of research and policy for the Canadian Centre on Substance Abuse.
"We tell people, well, you know you shouldn't get drunk. But what does it mean to drink responsibly? Does it mean not drunk?"
Health Canada is expected to issue in the new year responsible drinking limits that would essentially be the equivalent of Canada's Food Guide, for drinking.
After one to three drinks, skin flushes, the heart speeds up and people become more talkative. At four to six drinks, judgment is slower. People are giddy, and their coordination impaired.
It usually takes less for women to get drunk, because of their proportionately higher ratio of fat to water than men. It's worse over the holiday season, when women court anorexia to squeeze into cocktail dresses.
There's a critical third question -- Do you drink alone? -- that can indicate a cause for concern.
If you say yes to that question -- and if you also say that you drink to escape worries and to build up self-confidence -- you are an alcoholic, according to Johns Hopkins.
Heavy drinking, defined as five or more drinks on a single occasion for men and four or more drinks for women on a monthly or more frequent basis, is considered the strongest predictor that someone will get into trouble with alcohol.
Approximately 3.3 million Canadians are high-risk drinkers. Among youth, 46 per cent are drinking heavily at least once a month.
But doctors aren't asking patients about their drinking, waiting lists for publicly funded treatment programs are growing and most provinces don't pay for medications to treat heavy drinking. Meanwhile, the drain on the Canadian economy from lost productivity from sickness and premature death, health care and patrols for impaired drivers and other law enforcement costs was nearly $15 billion in 2002 alone.
A new national alcohol strategy makes 41 recommendations to move the country toward a "culture of moderation" and a new way of thinking about booze. The strategy calls for visible labels that list the number of standard drinks in each container of beer, wine or liquor, better screening for risky drinkers, improved access to addiction services, minimum retail prices for alcohol and public awareness campaigns.
So, are calls for a "nation of moderation" just a new cultural war, or a sort of puritan way of what the world should look like? The norms around alcohol have become tighter and tighter, says sociologist Ron Roizen. One sign? "Lower and lower levels of drinking have become defined as problematic."
Binge drinking, he says, has become institutionalized within the research industry as five drinks per sitting for men, four for women, "more or less independent of the length of the sitting, the size of the drinker and their experience."
"That is not what ordinary language regards as a binge. A binge is a protracted episode of drinking that may stretch across days with no periods of non-drinking, save for sleeping or unconsciousness.
"An awful lot of people are very light drinkers. Alcohol is used with remarkable temperance by most people who use it," Roizen says. "What is a 'problem' that's worthy of the public's concern? I don't think it's necessarily true that because people report that their wife gets angry with them about their drinking now and then that that's something public policy should be interested in."
Alcohol exists in virtually every segment of society in some form or another: beers at the hockey game, a toast to the bride. During the holiday season, "you can hardly go to any social function anywhere without there being alcohol," Beirness says. "Not that there's anything wrong with that. That's how ingrained it is. It's everywhere."
Not only is it available, there's an implicit expectation that you will partake, that you will drink.
"When we talk about a culture of moderation, that's where we have to make the changes, so that even if alcohol is there, you don't have to have any," Beirness says.
"Or, you can have one, or two. You don't have to have six."
-----------------------
The following simple test is used at Johns Hopkins University Hospital in Baltimore to help determine whether a patient is an alcoholic.
Answer yes or no to the following 20 questions:
1. Do you lose time from work due to drinking?
2. Is drinking making your home life unhappy?
3. Do you drink because you are shy with other people?
4. Is drinking affecting your reputation?
5. Have you ever felt remorse after drinking?
6. Have you ever had financial difficulties as a result of drinking?
7. Do you turn to lower companions and an inferior environment when drinking?
8. Does your drinking make you care less of your family's welfare?
9. Has your ambition decreased since drinking?
10. Do you crave a drink at a definite time?
11. Do you want a drink the next morning?
12. Does drinking affect your sleeping?
13. Has your efficiency decreased since drinking?
14. Is drinking jeopardizing your job or business?
15. Do you drink to escape from worries or troubles?
16. Do you drink alone?
17. Have you ever had a complete loss of memory as a result of drinking?
18. Has your physician ever treated you for drinking?
19. Do you drink to build up self-confidence?
20. Have you ever been to a hospital or institution because of drinking?
If you answer yes to any one of the questions, that is a warning you may be an alcoholic.
If you answer yes to any two, chances are you are an alcoholic
If you answer yes to three or more, you are an alcoholic.
How to get help:
If you need emergency help, go to your local emergency department or call 911.
Distress or crisis phone lines are open 24 hours a day if you need to talk to someone.
For a list of Alcoholics Anonymous meetings in Canada, go to www.aacanada.com.
For a list of Al-Anon/Alateen meetings for anyone whose life has been affected by someone else's drinking, go to www.al-anon.alateen.org. You can also call ![]()

![]()
![]()

![]()
![]()
![]()
![]()
![]()
![]()
![]() 1-888-4AL-ANON
1-888-4AL-ANON![]() (
(![]()

![]()
![]()

![]()
![]()
![]()
![]()
![]()
![]()
![]() 1-888-425-2666
1-888-425-2666![]() ) Monday through Friday, 5 a.m. to 3 p.m. To find local meetings, check the white pages of your phone book under Al-Anon.
) Monday through Friday, 5 a.m. to 3 p.m. To find local meetings, check the white pages of your phone book under Al-Anon.
source: CanWest News Service © The Vancouver Sun 2007
For addicts, holidays are tough, but sense of community can help
The shame of drink-driving
The Christmas anti-drink drive campaign is in full swing, but there will always be those who think they can get away with it. Beyond the points, the driving ban and the criminal record, how do those caught handle the shame?
Another Christmas, another warning about getting behind the wheel while under the influence of alcohol.
The theme of the 2007 campaign is that a conviction can ruin a driver's life. "That pint could come between you and Christmas" is the slogan.
The criminal record and driving ban are automatic and for those who rely on their cars that can be punishment enough. But what about the stigma and the shame?
Claire, a 27-year-old care co-ordinator from Torquay in Devon, found that being convicted even affected her relationship with her mother.
"She made me feel really, really bad. She didn't want to see me and shut the door in my face and told me to go away. That was the worst feeling ever."
Claire, which is not her real name, says the incident that changed her life came at the end of a "rubbish" day at work last year, close to the anniversary of her grandmother's death.
She began drinking a bottle of wine at home and then went into town to continue drinking, but on the way she hit a parked car, failed a breath test and spent a night in a police cell.
"That was lonely and horrendous. You feel very bad about yourself," she says.
Lessons
"It gives you time to think things over and how you could have killed someone. You feel embarrassed because you don't think you could ever end up in a cell."
She was given a £300 fine and a 16-month driving ban. The ban was reduced to a year because she signed up for a course with the Devon Driving Course run by Devon County Council, which aims to educate drink-drivers about their crime.
The court case meant she had to tell her parents the truth and endure her mother's cold shoulder, having previously told her the accident had not been her fault.
"I don't want people to make the same mistakes as I did. People's silence and the looks on their faces says it all. It makes you never want to do anything so stupid again."
She learnt many things from the £145 course but among them was the fact her shame, criminal record and costs could have been avoided had she paid £20 for a taxi.
While younger people like Claire have grown up bombarded by campaigns warning of the dangers, the middle-aged experienced no such media crusade in their 20s.
Falklands War veteran Roger Fenton, 55, from Cornwall, was attending a reunion around the time of the conflict's 25th anniversary in May when he gave a friend a lift home.
Career 'over'
He was stopped by the police for not having his lights on and - being a salesman - he feared his career could be over when he was banned for a year.
"I had been with the company for 23 years so luckily they showed me similar loyalty and hired someone as a chauffeur," he says.
"But my boss said he wasn't surprised this had happened because he'd noticed how heavily I'd been drinking, and my wife said the same."
The conviction, and the driving course that followed, provided a wake-up about the quantities he was drinking.
"I was pretty disappointed with myself. There's a stigma attached to drink driving. I'm the oldest person at my work place, and I'm the idiot."
source: BBC News
60 MINUTES Investigates New Treatment
Addicts and doctors say it works, but a prominent addiction doctor says the Prometa Treatment is unverified and puts marketing before science.
An increasingly popular drug protocol that addicts and some doctors say has been effective in curbing drug and alcohol cravings is an unverified treatment that a former junk bond salesman is marketing through a loophole in federal drug regulations, several prominent addiction doctors say. One of them, Dr. John Mendelson, who specializes in addiction medication, tells Scott Pelley that the treatment, called Prometa, has little science to back its claims in a 60 MINUTES report to be broadcast Sunday, Dec. 9 at 7:00 PM on WFMY News 2.
Prometa is touted as new treatment for methamphetamine, cocaine and alcohol addiction. It is a combination of three drugs already approved by the FDA. Mendelson says none has been proven effective individually against addiction. Could there be something special about taking them in combination? "So far, the evidence would suggest no," says Mendelson, who tests addiction treatments for the National Institute on Drug Abuse. What's special, says Mendelsohn, is the way its marketers have sold Prometa. "Their pathway...has been to...open Prometa centers so they can...dose people in their special clinics," he tells Pelley, "and to stay completely outside the scientific and regulatory framework."
The Prometa treatment did not have to pass muster from the FDA because all three of its drugs are already approved and their prescription by doctors for addiction - called off-label use - is perfectly legal. Mendelson wants more scrutiny. "They're just saying this stuff works without actually subjecting it to the proper kinds of trials," says Mendelson. "It is shocking. I've never seen anyone actually try it...this is one of those loopholes that may exist because no one has had the chutzpah to go out and actually try it...up until now," Mendelson tells Pelley.
Terren Peizer is the man who tried it. He raised $140 million to market Prometa, which can cost private patients up to $15,000. The former bond salesman, who once worked for junk-bond king Michael Milken, and his investors will make millions if they can persuade the health insurance industry and the government to accept Prometa. The regimen works and that's the important thing, Peizer says. "You could talk to 100 doctors out there using it. You could talk to 2,000 patients using it," he tells Pelley.
60 MINUTES did talk to doctors who say they've seen results with Prometa. Dr. Matthew Torrington, a former addiction researcher who directs the Prometa Center in Los Angeles, tells Pelley how it worked for one patient. "It wasn't like he couldn't remember cocaine anymore. It was that cocaine went from all he could think about to being just another thing on the list." Dave Smart, who says he was addicted to methamphetamine for 20 years, puts it another way. "The cravings were gone. I mean, overnight. That's the way it worked for me," he tells Pelley. "I never would have believed it. You're right, but it happened," says Smart.
Still, researchers are dismayed over the marketing process and the fact that no independent test on the treatment has been done. There is a placebo-controlled, double-blind study under way that will apparently support some of Prometa's claims, but it was run by a researcher who also owns an addiction clinic that uses Prometa, among other treatments. He denies there is any conflict. In addition, the 2006 annual report for Hythiam, Peizer's company, says that four other double-blind clinical studies of Prometa are underway: two in Los Angeles at the University of California and at Cedars -Sinai Medical Center; one at Medical University of South Carolina; and one at the Institute of Addiction Medicine at the University of Pennsylvania.
Another potential impediment seems to be that supporters of the treatment sometimes have bought its company's stock. That conflict of interest, coupled with an auditor's finding that Prometa was no better than other treatments, was enough for a county addiction program in the state of Washington to discontinue funding for Prometa.
Told by Pelley that to some he's a revolutionary and to others he's selling snake oil, Peizer replies, "Let the patients decide. If [Prometa] shows dramatically better results, shouldn't every state be using it to get patients better...lower healthcare costs....Isn't that what it's really about?" he asks. "So, snake oil? I think not," he tells Pelley.
Source: CBS and WFMY News 2
Copyright: 2007 digtriad.com
Early detection of alcohol dependence
One of the disadvantages of early detection of alcohol dependence is that it makes medical personnel think of physical damage first, where as social problems such as marital breakdown or loss of job are earlier indicators. These are often followed by psychological difficulties such as depression, anxiety or change in personality. Physical disorders generally occur later. Alcohol induced gastritis, ulcer pain, vomiting of blood and cirrhosis are the common medical problems. Alcohol related problems may occur singly but the more and longer an individual drinks the more problems he risks. An alcohol dependent person displays the following main features:
* The dependent drinker drinks to reliever or avoid withdrawal symptoms and drinking increasingly takes priority over other activities.
* The development of tolerance is shown by the dependent person being able to sustain an alcohol intake which would incapacitate the average man. For example, blood alcohol concentration of 300 mg% does not indicate a person’s manly ability to hold his drink, but rather his pathological tolerance.
* The dependent drinker becomes liable to withdrawal symptoms after 8-12 hours of abstinence. Each morning he may experience tremors, which varies from shaking of the hands to the whole body, nausea or vomiting, sweating, itching, muscle cramps and mood disorders.
* These withdrawal symptoms are temporarily ‘cured’ by drinking more alcohol. The drinker finds he can no longer control his drinking or be sure of stopping once he has started and drinking after abstinence is likely to lead to reinstatement of the entire episode.
Because of the relatively poor results of treating the established and heavily dependent drinker, emphasis has recently turned towards prevention and early detection. Alcohol related problems are caused by many causes and research has implicated a variety of predisposing factors such as heredity, personality and occupation.
Overall, per capita consumption is related to the price and availability of alcohol. Wherever alcohol is relatively cheap and widely available (as in Sri Lanka), the per capita consumption is high and alcohol related problems are common. Since governments control the price and availability of alcohol, the prevalence of alcoholism is both a medical but political problem. Psychologists and doctors are increasingly confronted with the social, psychological and physical consequences of excessive alcohol consumption
It is not difficult to diagnose the pot-bellied person who shakes as he breathes stale alcohol, but it is difficult to recognise the excessive drinker decades earlier.
There are at risk factors to recognise an alcoholic dependent person.
* Marital problems e.g. Violence towards the family.
* Problems at work; repeated absence on Mondays.
* Problem drinkers are much more liable to accidents at home, at work and on the roads.
* A relative with alcoholism-alcoholism is a family disease.
* High risk occupation; commercial travellers, company directors, entertainers, journalists, soldiers, and doctors.
* Mental disorders anxiety, depression and attempted suicide.
* Physical disorders; gastritis, liver disease.There are some blood tests which will show whether a patient is alcohol dependent.
There are psychological treatment such as aversive therapy and behavioural modification therapy to treat alcohol dependents. These therapies are effective, but takes a long time to produce the expected results.
source: The Island











